Summary of the NDIS Survey: We listen, we act, we care.
September 2025
In July of 2025, APodA conducted a survey to explore the potential impacts of the NDIS Pricing Arrangements introduced on 1 July 2025. We have now compiled the findings into a report which can be read below or PDF downloaded.
1. Introduction
The following report outlines the response of APodA members to the 2024-2025 NDIS Annual Pricing Review recommendations and the impacts to podiatry.
2. Background
On 11 June 2025 the 2024-2025 NDIS Annual Pricing Review was released and recommended the following changes:
- Changes to the podiatry fee from 193.99 per hour to $188.99 per hour. A reduction of $5.
- A 50% reduction in the travel fee (half the hourly rate) for time spent travelling to appointments e.g. can claim 50% of $188.99 which is $94.50.
The Australian Podiatry Association (APodA) immediately advocated along with other allied health organisations for the price cuts to be halted and reviewed. Advocacy included a snap poll, which ran from June 12-17 and provided initial reactions from the podiatry community on what the changes would mean for them. This information assisted in messaging and advocacy engagement. Further information on how APodA is advocating can be accessed on the NDIS advocacy page.
On 16 June and less than a week later the 2025-26 NDIS Pricing Arrangement and Price Limits were released. The new pricing arrangements were introduced as planned by the NDIS on 1 July 2025. To gauge general sentiment the APodA launched a survey which is the focus of this report. Refer to Appendix 1 for a copy of the survey.
3. Methodology
The development of a more in-depth survey was guided by the responses to the snap poll and input from the podiatry community. The survey was developed using Microsoft Forms and distributed directly to APodA members working in the NDIS. To boost engagement, it was also promoted through social media and through a pop up on the APodA website. The survey was launched on 19 June and closed on 29 July.
4. Results
Eighty-five (85) podiatrists completed the survey which provided both quantitative and qualitative information. Overall, the results showed that there is anger and frustration in the podiatry community. Overwhelmingly podiatrists care about NDIS participants, and want to be valued and paid fairly for delivering therapy supports.
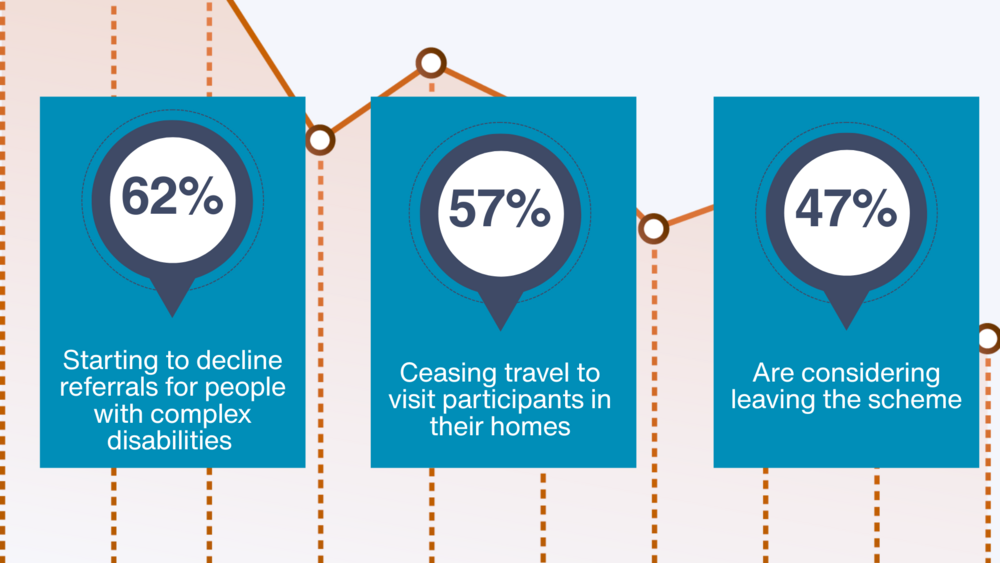
Podiatrists indicated the action that they intended to take because of changes to the NDIS:
- 62% starting to decline referrals for people with complex disabilities
- 57% ceasing travel to visit participants in their homes
- 47% considering leaving the scheme
5. Key themes
Podiatry professionals play a vital role in supporting NDIS participants by:
- Enhancing mobility and independence
- Preventing hospitalisations
- Managing complex conditions
Podiatrists consistently describe the work with NDIS participants as deeply rewarding, citing the complexity and diversity of cases as a source of professional fulfillment. However, this sense of purpose is increasingly overshadowed by systemic and financial challenges that threaten the sustainability of their involvement in the scheme.
Podiatrists are calling for transparency in decision-making, especially regarding fee structures and funding cuts. There is frustration over the lack of consultation and perceived disconnect between policymakers and frontline workers.
The following themes reflect the responses received.
5.1. Financial viability and remuneration
Podiatrists are calling for an increase in fees—not cuts—to support their work with NDIS participants. Concerns include:
- Reduced pay for services and travel, especially amid rising inflation and cost of living.
- Lack of fee increases since 2019.
- The current funding model does not reflect the true cost of care, particularly for home visits, complex cases, the high cost of providing podiatry care and administrative tasks.
“Reconsider the pay cuts. NDIS participants have complex needs and require allied health services provided by passionate, experienced, knowledgeable and dedicated clinicians. Allied health care workers deserve to be paid a fair remuneration. Without this level of care, the burden will fall on our already overburdened public hospitals.
“We are not asking for more funding just it be indexed to inflation rates”
“Participants in the NDIS are typically more complex than those in other schemes. This requires the upkeep of different skills & training from varying diagnosis & conditions, mental health & behaviours, not to mention keeping informed on regulatory compliance in order to maintain best practice in care provision and within the NDIS framework. “
- The recent changes to travel fees are expected to significantly impact service delivery, particularly in rural regions where home visits are often the only viable option.
“Travel to these Participants home and community environments is often essential, this comes with more overheads than typical MBS & PHI models, not to mention longer consultation times that result from providing services in these environments.”
Many clinics report that they could cease NDIS services without financial loss, as private clients offer higher returns with less administrative burden.
5.2. The benefits of working with NDIS participants
Podiatrists are passionate about working with NDIS participants, finding their work both challenging and rewarding
“The NDIS is such a monumental, life-changing scheme. All of Australia wanted this to work. It had the capacity to really respect people with disabilities and make their lives more meaningful and fulfilling. It was the first scheme of its kind in the world. It was revolutionary.”
“Working with NDIS participants is the most rewarding part of my job. The complexity and challenges associated with each individual makes it a more inspiring space to work in.
5.3. Administrative burden and systemic inefficiencies
The fragmented structure of the NDIS—with multiple plan managers and coordinators—creates confusion and inefficiencies in billing and service delivery.
Providers face:
- Excessive administrative requirements
- Inconsistent expectations from plan managers
- The cost of maintaining accreditation and compliance, especially for smaller practices and in regional areas.
“NDIS needs to be a simple scheme where the client is the priority.”
“It’s expensive to become and stay a registered provider.”
“Simplify the NDIS system. Acknowledge our registration board and therefore reduce the red tape for qualified and board certified professionals”
Despite being trusted allied health professionals, podiatrists feel the system treats them with undue suspicion.
5.4. Undervaluing of podiatry
Podiatrists want recognition for the critical role they play in supporting NDIS participants with complex needs.
Issues include:
- Podiatry often being excluded or not prioritised in participant plans despite its critical role in preventing hospitalisations and reducing the impact of disability
- Lack of understanding by the NDIS of podiatry scope and value
- Participants being redirected to public health systems, through Medicare or expected to self-fund their treatment
“We need to increase recognition of podiatry’s scope in the treatment and prevention of age-related diseases, complex disabilities.”
“We have a large, helpful role to play in preventing hospitalisations.”
5.5. Ethical tensions and workforce impact
Podiatrists are caught between ethical obligations to deliver quality care and the economic realities of running a practice.
Many express disillusionment and are considering withdrawing from the NDIS, despite their passion for working with this population.
“Podiatry clinics are busy enough as it is. We could cease seeing NDIS participants and still be booked out weeks in advance. It’s less money and more work that we don’t actually need. I’m confident a lot of clinics feel the same. Unfortunately, that means NDIS participants may struggle to find podiatry care in the future.”
6. Conclusion
Podiatrists are passionate about supporting NDIS participants and believe in the scheme’s transformative potential. However, without urgent reform, the sustainability of podiatry services—and the wellbeing of participants—are at risk.
There is a strong consensus that the NDIS needs structural reform, including:
- Fair and evidence-based pricing
- Streamlined administrative processes
- Greater recognition of allied health roles
- Integration with public health systems to ensure equitable access to essential services
Appendix 1: NDIS Survey Questions
1. Please tell us the impact that this will have on you as a practitioner and the participants in the scheme that you provide services for.
- I will start declining referrals for people with more complex disabilities
- I will stop traveling to visit participants in the scheme
- I will consider leaving the scheme
- I will continue to provide NDIS services as normal
2. So that we can understand the real world impact of the changes on NDIS participants, how many NDIS patients would you be treating in a given year?
3. If you are considering leaving the scheme is it because of (tick all that apply):
- Administrative burden
- Unpaid work required to liaise with support coordinators/plan managers to arrange services that are needed
- Poor payment processes
- Excessive reporting
4. How does working in the NDIS compare to working in MBS? (tick all that apply)
- Billing is easier in MBS
- GP looks after arranging services/care coordination
- Reporting is easier in the MBS
- Consumers are less complex in the MBS
- Working in the NDIS is the same as MBS
- Working in the NDIS is easier than the MBS
5. How does working in the NDIS compare to working in private health insurance (PHI)? (tick all that apply)
- Billing is easier in PHI
- GP looks after arranging services/care coordination
- Reporting is easier in the PHI
- Consumers are less complex in the PHI
- Working in the NDIS is the same as PHI
- Working in the NDIS is easier than the PHI
6. Do you have any other comments that you would like to make about working in the NDIS?
7.If you were talking to the Prime Minister today, what would you ask for?
8. Would you be prepared to help with developing participant stories to demonstrate the impact including the potential for adverse complications such as amputations?
- Yes
- No
